The Vascular System
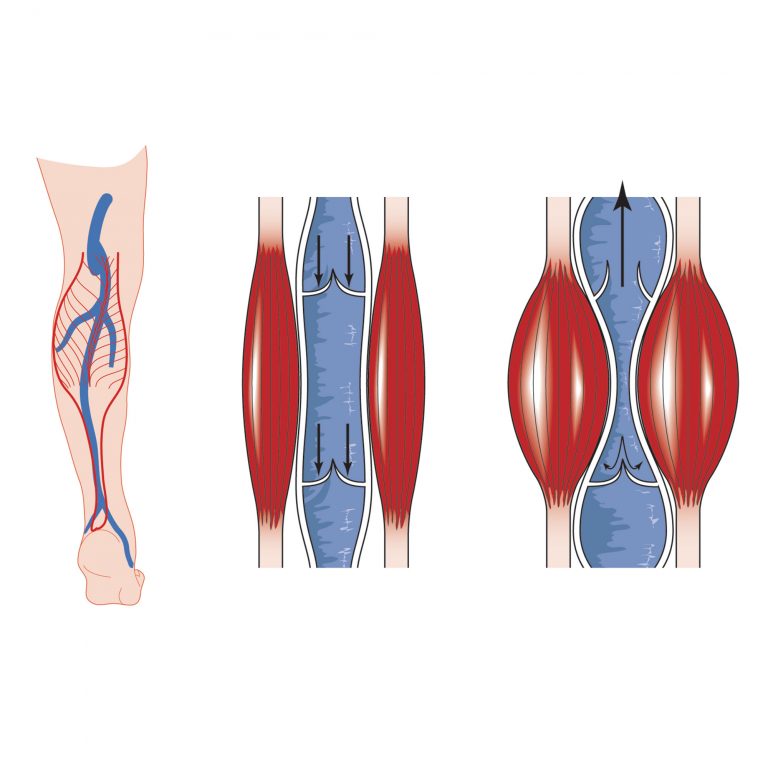
The human vascular system is composed of three main parts: the arterial system, the venous system and the lymphatic system. While arteries carry oxygen to cells, veins carry deoxygenated blood back to the lungs and heart. Veins are elastic and unlike arteries, depend on one-way valves and muscle contractions to propel blood back toward the heart against the pull of gravity. Calf muscle contractions, such as when walking, are especially important in moving blood through the veins of the legs. This is called the “calf muscle pump.” Medical Compression Stockings (MCS) work in tandem with the calf muscle pump to improve circulation.