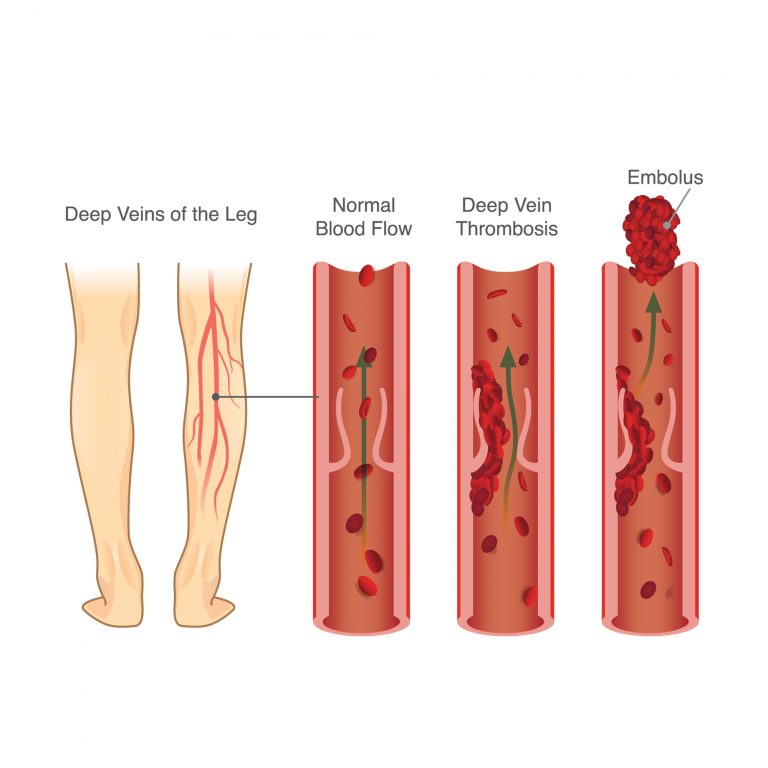
What is a DVT?
Deep Vein Thrombosis (DVT) is commonly referred to as a blood clot. Chances are you know someone who has had a blood clot or you have had one yourself. A DVT can happen to anyone at any time and affects millions of people worldwide. If left untreated, it may cause serious complications or even death. Wearing Medical Compression Stockings (MCS) and staying active is an important step in reducing your risk of a DVT.